Psoriasis is an auto immune disease that causes the skin cells to reproduce at a rapid rate. Normal skin cells grow and shed in a one-month cycle but with psoriasis, this process takes place over 2-3 days which subsequently causes thick, itchy, sore and often inflamed patches on the skin and scalp. The root causes of this debilitating disease is widely known to be rooted in an error of the immune system, however, genetics (one third of psoriasis sufferers have a relative that has it), diet, environment and social factors are also reported to be common causes for the onset of psoriasis. To make things worse, there are 5 main types of psoriasis and the symptoms of each of these can affect more than just the skin. With no cure or single treatment for psoriasis available that works for everyone, it is important to find out which type of psoriasis you are experiencing, look at all the information available and then find a way to adjust your lifestyle to reduce the symptoms as much as possible.
PLAQUE PSORIASIS

If we start here, we will cover about 80% of psoriasis sufferers psoriasis as most people who are diagnosed with psoriasis have plaque psoriasis, either alone or in combination with another type such as nail psoriasis (discolouration, pitting or separation from the nail bed) or psoriatic arthritis. Plaque psoriasis gets its name from the ‘plaques’ that are formed by the build-up of skin cells.
SYMPTOMS
Plaque psoriasis causes thick, raised, scaly patches of skin to develop. These scaly patches often form on the elbows, knees, and scalp, and can last for weeks, months, or years. On skin of colour, plaques may appear darker and thicker and would be a darker brown or greyish colour. Other symptoms include itching and burning skin, thickened or ridged nails, stiff and swollen joints.
TRIGGERS
Common triggers for plaque psoriasis include:
- Certain medications
- Starting or stopping medicines
- Infections
- Injury to the skin
- Stress
- Tobacco or alcohol use
TREATMENTS
Treatments are varied but include phototherapy, biologics, vitamin D creams, corticosteroids, diet changes, herbal creams and ointments Steroids are commonly used to treat mild to moderate psoriasis. It works by slowing down the production of skin cells and reducing the itching. Steroids will mostly just suppress the symptoms and withdrawing from them can cause what is known as a ‘healing crisis’ which could manifest as a full-blown flare up. Many sufferers are turning to more natural topical products such as M-Folia treatments and are taking steps to change their diet and lifestyle to reduce and minimise the symptoms of psoriasis.
GUTTATE PSORIASIS

The name guttate psoriasis comes from the Latin word guttate,
which means “drop” – this is mainly because of the raindrop or tear shaped small, red scaly patches that are the main characteristic of this type of psoriasis. It is the second most common type of psoriasis and can develop very suddenly, often after an infection such as strep throat. It generally starts in children or young adults and there’s a good chance it will disappear completely after a few weeks, but some people go on to develop plaque psoriasis.
SYMPTOMS
Unlike the thick, silvery scales that develop in plaque psoriasis, the lesions in guttate psoriasis are much smaller and thinner with several hundred of these drop shaped patches appearing on areas all over the body including the scalp and face. Usually the palms of the hands and soles of the feet are not affected.
TRIGGERS
It is still not known why the immune system overacts the way it does or why it comes on so suddenly, but there are various triggers that can start a guttate psoriasis flare. These include:
- upper respiratory infections
- streptococcal infections
- Tonsillitis
- Stress
- Skin Injury
- Certain medications
- Hormonal disorders
- Genetics
- Excessive Alcohol
TREATMENT
Mild guttate psoriasis requires topical medications as a first step in order to moisturise the skin and relieve the itching. Often steroid creams and ointments are prescribed but vitamin D treatments and other natural, herbal creams and gels are often very effective. M-Folia contains Mahonia Aquifolium which is an extract proven to have anti bacterial and anti fungal properties that will ease itching and soreness very quickly on the body and scalp.
Other treatments include:
- Phototherapy with ultraviolet light
- Antibiotics to treat strep throat
- Baths with Epsom Salts or Dead Sea Salts
PUSTULAR PSORIASIS

Pustular psoriasis is a rarer type of psoriasis that causes pus-filled blisters (pustules) to appear on your skin. It is not contagious and around 1 in 10 people with pustular psoriasis have a previous history of plaque psoriasis. It is very rare in children and usually occurs a bit later in life.
Pregnant women can develop this type of psoriasis despite never having had psoriasis before. The hormone changes, mostly in the third trimester, affect the immune system, however this usually disappears after the pregnancy. It is known as impetigo herpetiformis and is a very rare form of pustular psoriasis.
SYMPTOMS
Pustular psoriasis can occur very suddenly with a range of symptoms that occur in succession. The skin will become hot and tender and small pustules will start to appear. These pustules will start to join together and pools of pus will form. The pus consists of white blood cells and is not a sign of infection. Once the areas of pus dry out, there will be a smooth, shiny surface left behind. This is a cycle and can reoccur every few days or sometimes weeks but it will eventually clear with the right treatment. As with all types of psoriasis there are triggers that can set off another flare at any time. Pustular psoriasis can be very painful and be accompanied by fevers, intense itching, nausea, muscle weakness and dehydration.
TRIGGERS
- the use of or withdrawal from certain internal medications, including corticosteroids
- overexposure to UV light, for example, sunlight
- Certain drugs i.e. penicillin, lithium, ibuprofen
- Stress
TREATMENTS
As with all types of psoriasis, it is so important to look at your lifestyle choices and take steps to reduce the symptoms or the frequency of the flare ups. Removing alcohol, nicotine, red meat, and acidic forming foods. Reducing stress and keeping your weight and fitness in check. These are all tools for coping with psoriasis symptoms. Pustular psoriasis is often more serious and will usually require medical treatment or hospitalisation.
BIOLOGIC THERAPY
People who experience frequent flares, or have moderate to severe symptoms, may be recommended to use a biologic treatment. This is administered either as an injection or an infusion. Biologics are known to help the underlying problem by targeting specific genes.
NATURAL REMEDIES
Pustular psoriasis usually needs medical treatment, but remedies such as bathing with salt water or oatmeal, using oil-rich moisturisers, applying natural topical treatments like m-folia and removing scales with a very soft cloth may offer additional relief by soothing the skin and relieving irritation and itching.
Blistering increases the risk of bacteria entering the skin, so keeping the skin clean is essential to reduce the risk of infection.
INVERSE PSORIASIS

Inverse psoriasis affects the skin folds on the body. It is often known as hidden psoriasis or intertriginous psoriasis and about 25% of people living with psoriasis develop it. It mostly occurs where skin is rubbing against skin in areas like the armpit, the groin, the inner thigh, under the breasts or between the buttocks. Most sufferers of inverse psoriasis already have plaque psoriasis on other parts of the body, but moisture (in the form of sweating) and friction create the perfect environment to trigger the symptoms for inverse psoriasis. It is often worse for people who are overweight as there is excess skin and deeper folds for the lesions to grow.
SYMPTOMS
Inverse psoriasis is different from other forms of psoriasis. There are no pus-filled spots or large scaly areas. Instead, there is a smooth, red, shiny rash which is not raised or dry and crusty. These inflamed rash patches are often moist to touch and can be highly irritated and itchy. They often cover large areas inside the skin folds. Because Inverse psoriasis is made worse by friction and sweating, it can be particularly uncomfortable in hot weather.
TRIGGERS
Common triggers for inverse psoriasis include:
- Starting and stopping medicines
- Infections
- Injury to the skin
- Friction on deep skin folds
TREATMENTS
Options usually include topical cream or systemic medications. It is essential to keep the lesions in the skin folds dry so using a powder is often recommended. Areas in the skin folds can be prone to fungal infections so medication to treat this may be prescribed. Weight loss and cool temperatures will keep the sweating and friction to a minimum and ease the itching and soreness.
ERYTHRODERMIC PSORIASIS
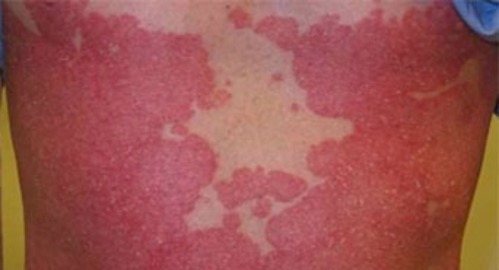
Erythrodermic psoriasis is a rare and dangerous form of psoriasis that affects only 2% of people living with psoriasis. It is aggressive and inflammatory, covering nearly all the skin on the body. This causes severe itching or burning and can be life threatening. Erythrodermic psoriasis disrupts the body’s normal temperature and fluid balance which can lead to intense shivering and possible swelling in areas such as the feet or ankles.
SYMPTOMS
This is the most severe type of psoriasis and spreads very quickly. Symptoms will include:
- Severe redness/discoloration over a large area of the body
- Skin shedding in large “sheets” instead of smaller scales
- Skin looks burned
- Increased heart rate
- Severe itching and pain
- Erratic body temperature
TRIGGERS
Erythrodermic psoriasis can develop over time but often happens very suddenly. Common triggers are:
TREATMENTS
As the most dangerous of all the psoriasis types, it is most likely that people with the symptoms of erythrodermic psoriasis will be taken straight to hospital. No doubt medications will be administered that will be effective in controlling an attack of out-of-control immune cells. Immuno-suppressing drugs or medicines that can control cell growth are the most likely to be prescribed by Doctors.
- To soothe your skin from the outside, you can use:
- Steroid cream or ointment moisturizers
- Wet wraps
- Oatmeal baths
- You may also need antibiotics to prevent any infection. Certainly you will be prescribed pain medication and something to control the itching.